The Challenges in Traditional CDI
- Time-Consuming Processes: Clinicians spend a substantial amount of time documenting patient encounters, upwards of 2-4hrs/day, often leading to burnout.
- Incomplete or Inconsistent Documentation: Missing clinical details can lead to coding errors, revenue loss, and suboptimal patient care.
- Regulatory Compliance Issues: Ensuring documentation aligns with ICD-10, CPT, and other regulatory standards requires constant vigilance.
- High Manual Review Workloads: CDI specialists and coders manually review and clarify documentation, leading to inefficiencies and delays.

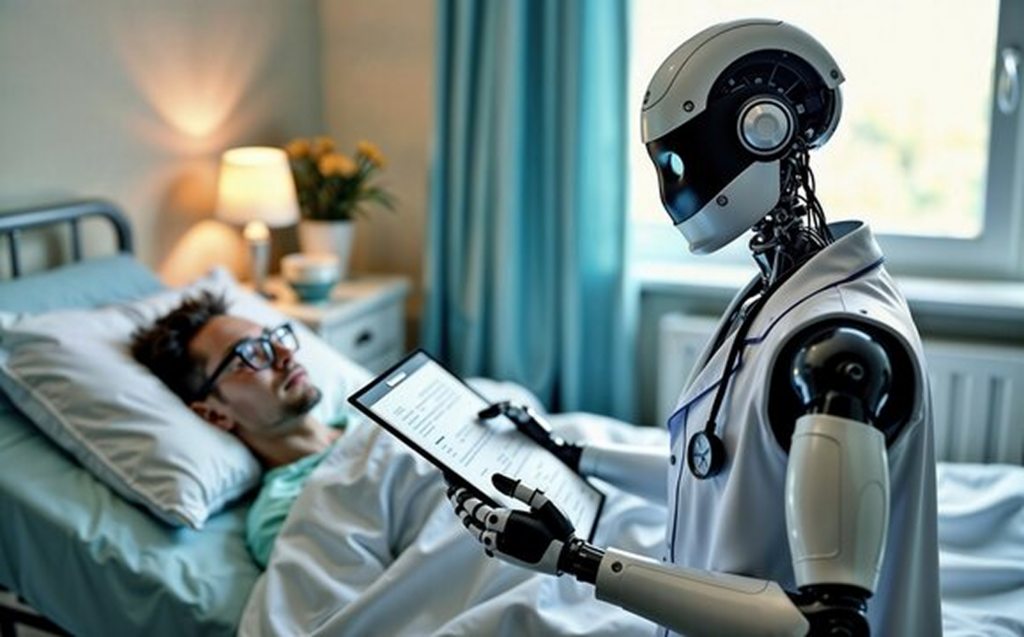
How AI is Enhancing CDI
1. Automated Clinical Note Generation
AI-powered LLMs, trained on vast amounts of medical literature and clinical notes, can automatically generate high-quality documentation from clinician-patient interactions. CARE-E takes this a step further by leveraging NLP to extract relevant details from voice recordings or structured data and generate comprehensive notes aligned with standard coding practices.
2. Real-Time Documentation Assistance
LLMs embedded into EHR systems can assist clinicians by suggesting real-time improvements, flagging missing details, and ensuring terminology consistency. AI-driven CDI tools like CARE-E can:
- Highlight missing diagnoses and procedures.
- Suggest appropriate ICD-10 and CPT codes.
- Prompt for additional documentation to improve specificity.
3. AI-Powered Clinical Validation and Auditing
NLP-based algorithms can analyze vast amounts of clinical data to detect inconsistencies or potential documentation gaps. CARE-E can:
- Identify contradictions between physician notes and lab results.
- Flag discrepancies in medication administration records.
- Alert CDI specialists to cases needing clarification before billing.
4. Enhanced Compliance and Risk Adjustment
CARE-E ensures that clinical documentation meets compliance standards by:
- Automatically mapping documentation to regulatory requirements.
- Identifying Hierarchical Condition Category (HCC) codes for risk-adjusted reimbursement.
- Preventing undercoding or overcoding by aligning documentation with payer policies.

5. Speech-to-Text and Conversational AI for Hands-Free Documentation
Advanced NLP models integrated with speech recognition enable hands-free clinical documentation. CARE-E allows clinicians to dictate patient interactions, transcribing and structuring the notes in real time to ensure completeness and accuracy. It also integrates with voice-based EHR navigation to streamline workflows.
6. Predictive Analytics for Proactive CDI
By analyzing historical documentation patterns, AI can predict potential areas of documentation deficiencies and recommend preemptive actions. CARE-E’s predictive models can:
- Identify high-risk cases requiring more detailed documentation.
- Provide CDI teams with insights on common documentation gaps.
- Assist in physician education by highlighting areas for improvement.
7. Structured Data Integration for Comprehensive Documentation
CARE-E enhances clinical documentation by structuring essential patient information from the patient encounter and EMR, including:
- Health Status Assessments (HSA)
- History of Present Illness (HPI)
- Past Medical History (PMH)
- Past Surgical History (PSH)
- Preventive Health Assessments (PHA)
- Orders (Medications, Labs, Imaging, Procedures, etc.)
- Treatment Plans
These structured data elements are seamlessly integrated into various clinical documentation formats, such as:
- SOAP Notes (Subjective, Objective, Assessment, Plan)
- ASPO Documentation (Assessment, Subjective, Plan, Objective)
- Discharge Summaries
- Patient Summary
- Referral Summary
By structuring this data in a standardized format, CARE-E ensures that patient records are comprehensive, easily accessible, and interoperable across different healthcare systems.

Real-World Impact of AI-Driven CDI
Hospitals and healthcare organizations adopting AI-enhanced CDI solutions like CARE-E have reported:
- 30-50% reduction in documentation time
- Improved reimbursement accuracy and reduced claim denials
- Increased compliance with regulatory standards
- Enhanced clinician satisfaction by reducing administrative burden
The Future of AI in CDI
As AI continues to evolve, the next generation of CDI solutions will likely leverage:
- Multimodal AI combining text, images, and structured data for deeper documentation insights.
- Advanced Large Language Models trained on real-world clinical datasets for highly contextualized recommendations.
- Federated Learning and Privacy-Preserving AI to ensure compliance with HIPAA and other data protection regulations.
By integrating AI-driven CDI solutions like CARE-E, healthcare organizations can enhance documentation accuracy, improve patient outcomes, and streamline revenue cycle management. As LLMs and NLP continue to advance, the future of CDI looks increasingly intelligent, automated, and efficient.
By Matthew Drew